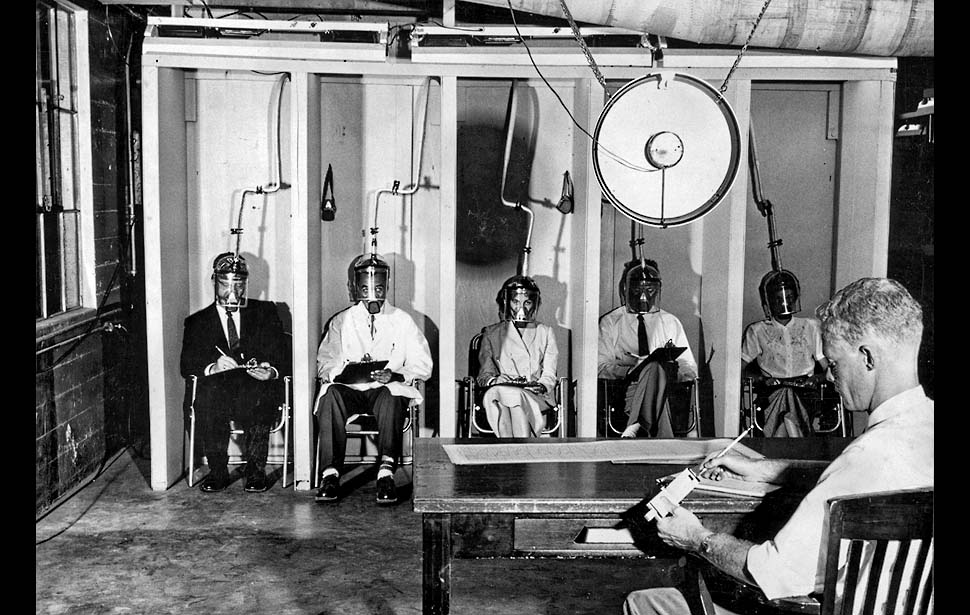
New research ethics guidelines planned for US
HHS has proposed an overhaul of existing human research ethics guidelines
The US Department of Health and Human Services (HHS) has proposed an overhaul of existing human research ethics guidelines in an attempt to deal with various advances in the sciences in the past two decades.
Earlier this month, the HHS published a Notice of Proposed Rulemaking (NPRM), setting forth suggested changes to the now outdated 1991 regulations (known collectively as the “Common Rule”).
The suggestions include proposals to modify informed consent for biospecimen research, improve the understandability of consent forms, mandate single institutional review board (IRB) oversight of research, and establish data security safeguards.
Many researchers and policy-analysts say that the existing framework is inadequate for studies involving new genomic technologies, and it also seems to hinder multi-site research.
Adil Shamoo, professor of biochemistry and molecular biology at the University of Maryland and chairman of the medical ethics subcommittee of the Defense Health Board, recently spoke out in favour of centralised Institutional Review Boards (IRBs): “I don’t believe in large bureaucracies,” he told Modern Healthcare.
“Cumbersome and outdated regulatory standards overwhelm and distract institutions, IRBs, and investigators in ways that stymie efforts to appropriately address the real risks and benefits of research,” the HHS notice reads.
The HHS wants informed consent to be required for secondary research with a biospecimen. The HHS understands this to include “part of a blood sample that is left over after being drawn for clinical purposes, even if the investigator is not being given information that would enable him or her to identify whose biospecimen it is.”
The proposed changes will have significant implications for a wide range of stakeholders across the life sciences and health care industries, including drug and device manufacturers, hospitals, academic medical centres, universities and medical schools, IRBs, contract research organizations, laboratories, and tissue banks.
Medical anthropologist Barbara Koenig is concerned about the effect on research into the screening of newborns for disease. She has studied the collection of samples from newborn babies, and says that “There’s a huge public benefit from the research done with de-identified samples.”
“Requiring explicit consent is going to throw a wrench in that.”
The HHS has begin a 90-day public comment period on the proposal and will decide how to proceed once that concludes.
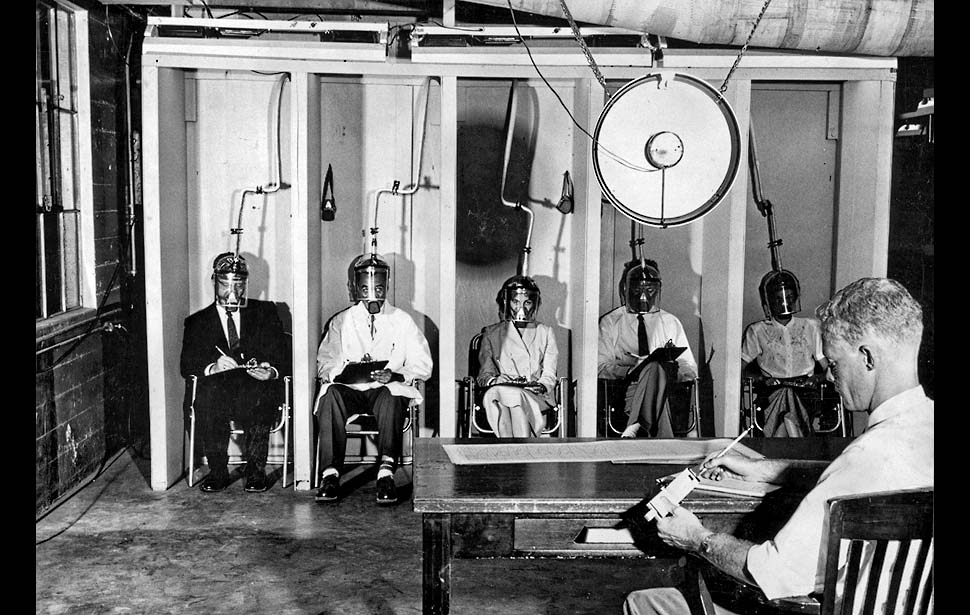
https://www.bioedge.org/images/2008images/TH_human_protection.jpg
Creative commons
https://www.bioedge.org/images/2008images/smogtest.jpg
Common Rule
research ethics
