
Desperate times call for … rationing conscience
Ever thought of conscience as a ‘resource’ to be ‘rationed’?
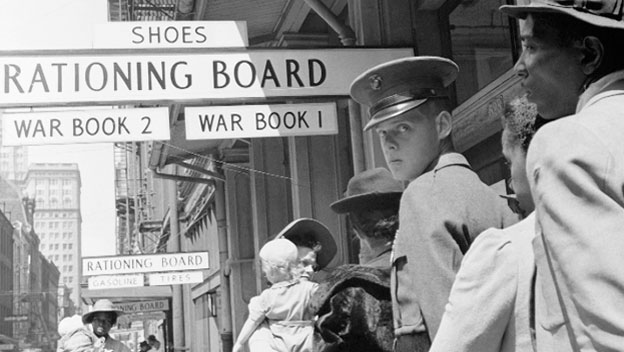
Bioethicists often look to the so-called ‘military analogy’ to understand conscientious objection in healthcare. Yet no one has gone so far as to suggest it is a ‘resource’ that can and should be ‘rationed’. At least, not until now.
In a paper published online first this week in Journal of Medical Ethics, Oxford ethicist Dominic Wilkinson suggests that we should place strict limits on conscientious objection in the context of the allocation of scare healthcare resources. While there may be certain circumstances where conscientious objection might be permitted, Wilkinson suggests there are strong arguments against allowing clinicians to disrupt the standard allocation of medical resources. Wilkinson states:
“[there are] substantial arguments against accommodating CO to allocation; such accommodation would almost always be inappropriate. Conscientious nontreatment or treatment run counter to fundamental principles of allocation including consistency, and the need to impose limits on available treatment.”
Wilkinson warns of a “‘roster lottery’ affecting the provision of potentially life-saving medical treatment”, and suggests “conscientious treatment” – the treatment of patients despite contrary State directives – could “potentially defeat the purpose of making community-level decisions about allocation and imposing limits on treatment.” Freedom of conscience paradoxically ends up looking like a scarce resource that must be carefully apportioned – at risk of disturbing a delicately balanced healthcare system.
Wilkinson, a neonatologist trained in Australia, was signatory to the recently released Consensus Statement on Conscientious Objection in Healthcare. Clause 2 of the Statement dealt with similar concerns to those expressed by Wilkinson:
“In the event of a conflict between practitioners’ conscience and a patient’s desire for a legal, professionally sanctioned medical service, healthcare practitioners should always ensure that patients receive timely medical care. When they have a conscientious objection, they ought to refer their patients to another practitioner who is willing to perform the treatment. In emergency situations, when referral is not possible, or when it poses too great a burden on patients or on the healthcare system, health practitioners should perform the treatment themselves.”
Desperate times call for … rationing conscience
Xavier Symons
https://www.bioedge.org/images/2008images/02_objection_conscience_1.jpg
Creative commons
https://www.bioedge.org/images/2008images/02_objection_conscience_1.jpg
conscience
conscientious objection
- Can machines be moral? - March 7, 2021
- Can we synthesise Christianity moral theology with secular bioethics? - November 28, 2020
- Euthanasia polling data may fail to capture people’s considered views - August 15, 2020
